Growing bacterial resistance in Gram-positive pathogens means that what were once effective and inexpensive treatments for infections caused by these bacteria are now being seriously questioned, including penicillin and macrolides for use against pneumococcal infections and—in hospitals—oxacillin for use against staphylococcal infections. As a whole, multidrug-resistant (MDR) Gram-positive pathogens are rapidly becoming an urgent and sometimes unmanageable clinical problem. Nevertheless, and despite decades of research into the effects of antibiotics, the actual risk posed to human health by antibiotic resistance has been poorly defined;
Antibiotic resistance is now acknowledged as a major public health issue, affecting virtually all major bacterial pathogens and spreading to all types of nosocomial settings as well asthe community at large.
Resistance is now documented in bacteria that, traditionally, were fully susceptible. In addition, multidrug-resistant (MDR) bacteria have risen to prominence, and new ‘opportunistic’, and often MDR, organisms are recognized increasingly as important pathogens in both the nosocomial and community settings.
Europe has been at the forefront of efforts to study and control antimicrobial resistance, and this has prompted numerous recommendations for action at both national and international levels.
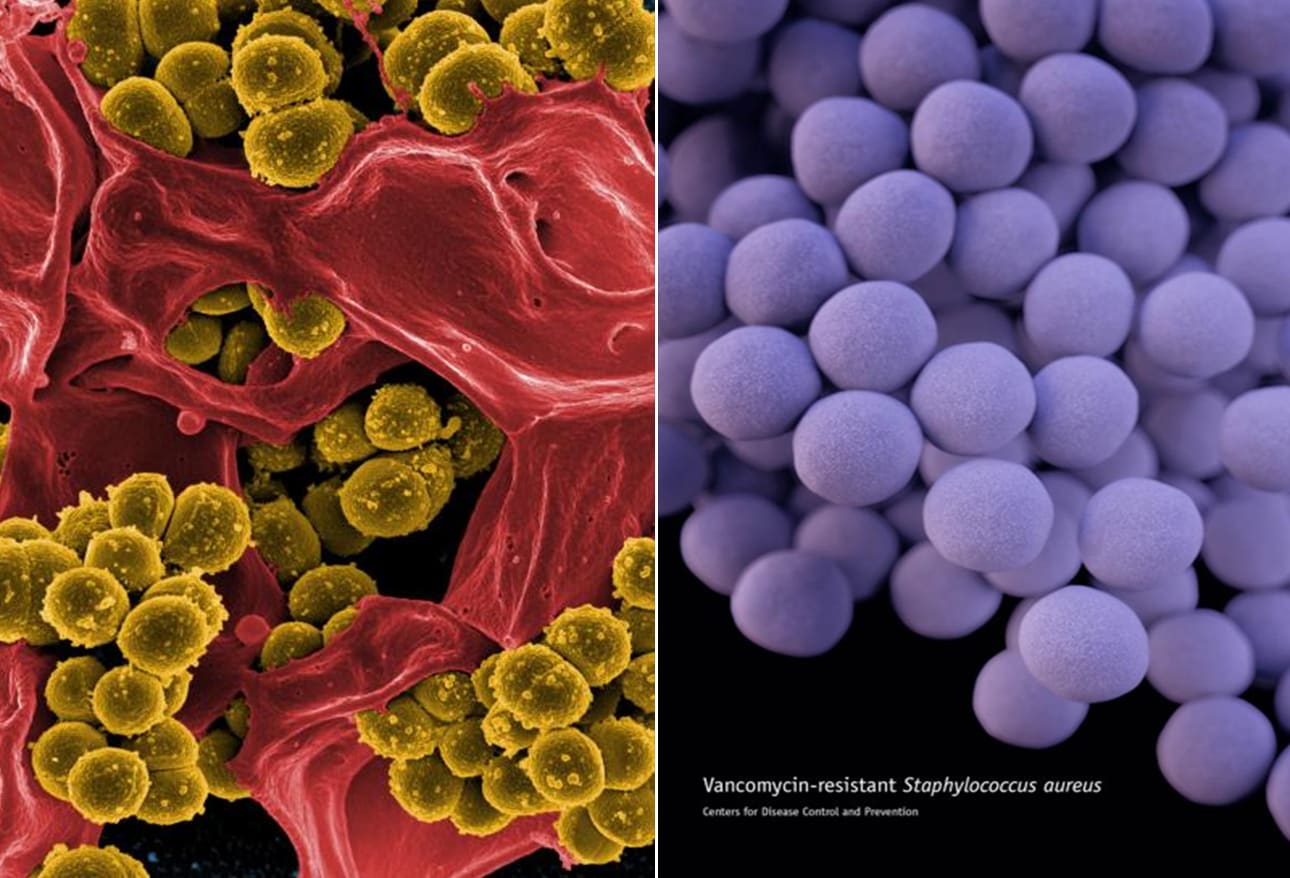
One of the major therapeutic challenges is, without doubt, multidrug resistance in Gram-positive pathogens. Multidrug resistance problems are related, at least in part,to the international dissemination of epidemic clones that have accumulated several resistance traits through an evolutionary process. Numerous molecular epidemiological surveys have outlined the widespread expansion in Europe of antibioticresistant clones of Gram-positive organisms such as penicillinresistant pneumococci, methicillin-resistant Staphylococcus aureus (MRSA), and vancomycin-resistant enterococci. The international spread of MRSA in hospitals is a major concern, widely echoed even in the lay press.
Recently, considerable epidemiological research has been directed at the spread of MRSA in the community setting also, arising independently of local nosocomial strains. Epidemiological data are also providing evidence of the growing importance of enterococci, and most notably Enterococcus faecium, as nosocomial pathogens, possibly following the expansion of the vancomycin-resistant clonal lineage CC17.
As far as pneumococci are concerned, the resistance trends vary throughout Europe for both penicillin and macrolide resistance, but a worrisome increasing trend towards dual non-susceptibility is being observed in many countries. Although the increasing diffusion of antipneumococcal vaccination is expected to affect the resistance picture dramatically, the potential for capsule switch among currently circulating invasive pneumococci must be seriously considered. Worthy of note is the fact that the new conjugate vaccine does not cover serogroups in which antibiotic resistance is quite common in Europe.
As a whole, MDR Gram-positive pathogens are rapidly becoming an urgent and sometimes unmanageable clinical problem, not only in pneumonology, oncology and urology wards, but also in intensive-care units. Mortality has increased among intensive-care patients, where infections are resistant to first-line and second-line empirical therapies. The presence of MDR Gram-positive bacteria has been variously associated with increased rates of re-operation, surgical site infection and abscess formation in intra-abdominal infections.
Surprisingly little is known, too, about the actual effectiveness of the many types of interventions aimed at controlling antibiotic resistance. Alongside a number of encouraging experiences in which interventions have been associated with a reduction in resistance rates, there is a lack of good-quality data indicating that widespread effects can be achieved or maintained. Researchers in the UK, who have systematically evaluated interventions to improve antibiotic prescribing in hospitals, found good evidence that reductions in antibiotic usage can reduce resistance in multiply resistant Gram negative bacilli. However, there is far less evidence of the effectiveness of these kinds of measures in controlling MRSA or vancomycin-resistant enterococci.