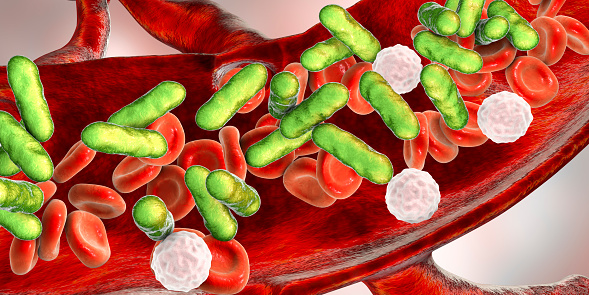
Blood transfusion has been and continues to be a possible source of disease transmission. A myriad of agents can potentially be transmitted through blood transfusions, including bacteria, viruses, and parasites. Of these, bacteria are the most commonly transmitted.
Viral agents that are capable of being transmitted through blood transfusion include the following:
Protozoal organisms that can be passed on through transfusion include species of the genus Plasmodium, which cause malaria.
Prions, which cause Creutzfeldt-Jakob disease, are also transmissible through transfusion; they cannot be destroyed using current techniques for inactivating pathogens in the blood supply.
Clinical features of TTBI
Although TTBI can produce a wide variety of clinical symptoms (including death), fever (>102º F, or a >3.6º F increase from the pretransfusion baseline), rigors, tachycardia, or an increase in heart rate by more than 40 beats per minute from the baseline and a fall of systolic blood pressure of greater than 30 mm Hg are highly suggestive of the condition. Chills and fever are the most commonly reported symptoms. Other clues include backache, abdominal pain, vomiting, and hypothermia.
As soon as TTBI is suspected, the following course of action should be taken:
In order to prevent an infective incident, strict sterile precautions and donor screening are required. Recommended measures include the following:
Viral Infections
Human immunodeficiency virus
The human immunodeficiency virus (HIV), a member of the Lentivirus family of retroviruses, is the causative agent of acquired immunodeficiency syndrome (AIDS). In the United States, more than 1.2 million people are living with HIV, and 1 in 8 of them don't know it. Individuals who engage in male-male sexual behavior accounted for 82% (26,375) of HIV diagnoses in men and 67% of all diagnoses in 2015. Less than 1% of HIV cases are attributed to blood or blood product transfusions.
Hepatitis B virus
The hepatitis B virus (HBV), a member of the Hepadnaviridae family, is capable of withstanding extreme temperatures and humidity. The viral genome consists of partially double-stranded, circular deoxyribonucleic acid (DNA) containing 3.2 kilobase (kb) pairs that encodes 4 overlapping, open reading frames.
Hepatitis B is a worldwide healthcare problem, especially in developing areas. An estimated one third of the global population has been infected with HBV. Approximately 300 million people are lifelong carriers, although annually, only 2% spontaneously seroconvert. In the United States, 300,000 cases of acute HBV disease are reported annually to the Centers for Disease Control and Prevention (CDC).
HBV is transmitted hematogenously and sexually. The outcome of this infection results from a complicated viral-host interaction that produces an acute symptomatic disease, an asymptomatic disease, or a chronic carrier state. Later consequences include cirrhosis and the development of hepatocellular carcinoma (HCC). Note: The residual risk of transmission of HBV is estimated to be close to 270,000 units in the United States and 1 in 70,000 to 1,000,000 units in various parts of Europe.
Hepatitis B surface antigen (HBsAg) detection is a routine in many parts of the world. However, some chronic carriers have such a low viral load that screening by HBsAg may not be able to detect the infection in the donor. To overcome this obstacle, many blood banks in several countries also attempt to detect antibody against the hepatitis B core antigen (anti-HBcAg or anti-HBc).The core antibody develops early in the course of the infection and remains positive even in patients with low-level viremia.
Hepatitis C virus
The hepatitis C virus (HCV) is a spherical, enveloped, single-stranded RNA virus belonging to the Flaviviridae family. The World Health Organization (WHO) estimates that 170 million individuals worldwide are infected with HCV.
HCV is predominantly transmitted by means of percutaneous exposure to infected blood. In developed countries, most new HCV infections are related to intravenous (IV) drug abuse and are found because of intensive screening and lookback programs.
Blood transfusion was a major risk for acute HCV infection in the past, with more than 10% of transfusion recipients acquiring the infection in some studies. The screening of blood donors by donor history and elevated serum alanine aminotransferase (ALT) caused a striking reduction of non-A, non-B posttransfusion hepatitis, even before HCV was identified. The subsequent initiation of donor screening for anti-HCV antibodies in 1990 nearly eliminated the risk of posttransfusion acute HCV infection.
Indeed, such screening has decreased the risk of transfusion-associated HCV infection to less than 1 case in 103,000 transfused units.
Protozoal Infections
Malaria
Malaria is endemic in many tropical and subtropical regions of the world. Over 300 million people worldwide are infected, with 1 million fatalities annually. The known causative agents are the following 5 species of Plasmodium:
Malaria is spread mainly through mosquito bites, but cases of transfusion-transmitted malaria have been reported. The risk of spread depends on the prevalence of the disease. For example, in Benin, where malaria is highly endemic, one third of screened blood donors were found to have P falciparum trophozoites, making them capable of transmitting the disease through blood donation.
In areas with a low prevalence of malaria, donors who are recent travelers or who are immigrants from endemic areas are potential sources for transmission of the infection. The FDA recommends that donors with a history of malaria be deferred for 3 years after becoming asymptomatic. Provided that donors are asymptomatic, travelers to endemic areas are deferred for 1 year after they return to the United States.
Trypanosoma cruzi
Trypanosoma cruzi is the causative agent of Chagas disease, which is generally spread by the bite of the reduviid bug. The illness has an acute and a chronic form. The acute form principally affects children in endemic areas, including Central and South America and parts of Mexico, and manifests as fever, lymphadenopathy, and hepatosplenomegaly. In severe cases, myocarditis and encephalitis may occur. The disease may take a more indolent course, however, and after a latency period of decades, it can present with serious end-organ damage, causing chagasic cardiomyopathy and megaesophagus.
Individuals from endemic areas may become chronic carriers of the T cruzi parasite and are responsible for transmission of T cruzi through blood transfusion. Such cases are well known in high-prevalence areas. Seroprevalence in the United States ranges from 0.12-0.20%, but only 7 cases have been reported to be transmitted by blood. Serologic testing and deferral of positive donors is a policy in endemic countries, and an enzyme-linked immunosorbent assay (ELISA)–based screening test has been instituted in the United States as well.
Inactivation of Pathogens
A desirable inactivation method would interfere the least with the function of blood products and yet be effective against infectious agents. Some of these methods are described below.
Solvent-detergent method
The solvent-detergent method is used to disrupt membranes of lipid-enveloped viruses without affecting the majority of plasma proteins, except protein S, antitrypsin, and antiplasmin. Hence, the method is effective in destroying HIV, HTLV, Epstein-Barr virus (EBV), HBV, and HCV. It is not effective against HAV and parvovirus; consequently, the blood product is tested for these 2 agents if the solvent-detergent method is used.
Loss of protein S, antitrypsin, and antiplasmin may occur during processes involving the removal of residual solvent detergent. This has been concerning in patients with hyperfibrinolysis, which occurs, for example, during the reperfusion stage of liver transplantation.
Methylene blue
Methylene blue is a dye that combines with cellular elements. Once it is exposed to light, the dye becomes active and disrupts the wall to which it is attached. This method has been used extensively in Europe to inactivate viruses. Limitations of the methylene blue technique include ineffectiveness against intracellular pathogens and likely interaction with coagulation factors. The loss of fibrinogen content is estimated to be around 20%, raising issues of efficacy when the treated product is used for plasma exchange in thrombotic thrombocytopenic purpura.