Despite antibiotic prophylaxis and the development of more refined surgical tecniques, microbial infection of the vascular prostheses are well known, not rare and redutable coplications.
The literature-reported incidence may vary between 0,2 and 5% and it is influenced by: the site of the implant, the underlying disease and the host defense mechanism.
Infection affects especially prosthetic grafts which are implanted during emergency procedures (for example emergency surgery for the ruptured abdominal aortic aneurysm) and prostheses anastomosed to the femorala artery or placed into an subcutaneous tunnel (for example the axillofemoral or axillobifemoral grafts).
Vascular graft infections are classified by their appearance time (early infections-which appear earlier than 4 months after graft implantation; late infections-which appear after 4 months), their relationship to the postoperative wound and the extent of graft involvement.
Szilagy’s classification is reffering to the grades of postoperative’s wound infection. So we have three
grades,as follows:
An early infection correlates with a Szilagyi grade III wound infection. These infections are caused by virulent hospital-acquired bacteria and present with sepsis signs like: fever, leukocytosis, bacteremia and easy noticeble signs of an infected wound (inflamated tissues around it, pus emerging from it).
Late infections are a result of graft colonization by “low-virulence” organisms such as: Staphylococcus epidermidis or Candida spp. They are characterized by the fact that they are indolent and have no signs of sepsis and cultures of the perigraft tissues are not growing any germs.
Pathogenesis of graft infection
The initiating event is the bacterial afherence to the biomaterial surfaces, followed by colonization and development of a bacterial biofilm that resist host defenses and antibiotic penetration.
The presence of a foreign body potentiates the infectivity of bacteria. Elek and Cone demonstrated in 1957 that a single-braided silk suture significantly reduced the inoculum of staphylococci recquired to produce a local infection. The risk of foreign body infection can be predicted by the formula:
Risk of biomaterial infection = (Dose of bacterial contamination× virulence)/Host resistance
Bacterial adherence to polyester grafts is 10 to 100 times greater than to PTFE grafts. Gram-positive bacteria produce an extracellular glycocalix made out of mucine which makes them much more adherent than, for
example, Gram-negative ones. Etiologic factors involved in graft colonization: perioperative contamination; bacteremia seeding of the biomaterial; mechanical erosion into bowel or genitourinary tract or through skin.
The risk factors for graft infection are:
Prevention
Vascular infections can be minimized if some simple principles are applied:
• avoid a prolonged preoperative stay to minimize the development of skin flora resistent to commonly used antibiotics;
• have patients shower or scrub with an antibacterial soap the night before the operation;
• control the remote infections before an elective operation;
• remove operative site hair immediately before surgery using scissors rather than razors, to minimize skin trauma;
• protect vascular grafts from contact with contaminating sources, especially the exposed adiacent skin, using iodine-impregnated plastic drapes or antibiotic-soaked towels;
• avoid simultaneous gastrointestinal procedures during garfting;
• use prophylactic antibiotics whenever a graft or stent is implanted;
• longer duration of perioperative antibiotics (>48 hours) may be considered whenever patients present more than two risk factors for wound infection, including extremes of age, malnutrition, chronic illnesses such as diabetes, remote infections or prior irradiation of the surgical site.
Antibiotic prophylaxis protocols for vascular procedures are as follws:
• Cefazolin 1-2 g IV slowly prior to induction of anesthesia and repeated (1-2g) each 8 hours for 24-48 hours, or cefuroxime 1,5 g IV and each 12 hours for a total of 6 g; a single dose of cefazolin 1 g IV is recommended prior to endovascular stent implantation;
• When MRSA (methycillin-resistant Staphylococcus aureus) is cultured from body surfaces or is a known important pathogen in hospitalized patients, add vancomycin 1 g IV infused over 1 hour;
• If the patient has a cephalosporin allergy, give aztreonam 1g IV each 8 hours for 24 hours;
• If the patient has a vancomycin allergy, give clindamycin 900 mg IV over 20-30 minutes followed
by 450-900 mg IV each 8 hours for 24 hours. In some vascular centers, prophylactic antibiotics are
continued for 3 to 5 days in patients being at high risk for infection from bacteremia, prolonged preoperative hospitalization or high institutional wound infection rates (>10%).
Bacteriology
S. aureus is the most prevalent pathogen, one fourth of prosthetic infections being caused by it. Lately, prosthetic infections caused by S. Epidermidis or Gram-negative bacteria have emerged. This change in the microbiology of graft infections is the result of reporting both early and late infections and of surgeons becoming more aware of the false-negative microbiological results taken from many late infections, owed to the low bacteria numbers present within the graft surface biofilm.
Garft infections associated with negative culture results are caused by S.epidermidis or other coagulase-negative
staphylococci, or by Candida species. Infections due to Gram-negative bacteria as E.Coli,
Pseudomonas, Klebsiella, Enterobacter and Proteus spp are very virulent.
The incidence of anastomotic dehiscence and artery rupture is high and is due to the ability of these organisms to produce destructive endotoxins. Fungal infections are very rare and most of the patients having them are immunosuppressed or have an established fungal infection elsewhere.
MRSA is responsible for one fourth of early graft infections, nowadays. This recent increase in MRSA graft
infections may justify the use of specific antibiotic prophylaxis for all vascular implant procedures.
Infection diagnosis is reached upon clinical examination, microbiology findings and intraoperative aspects.
Diagnosis
Clinical evaluation includes: patient history, physical examination and vascular imaging( arteriography,ultarsonography, contrast-enhanced CT, endoscopy).
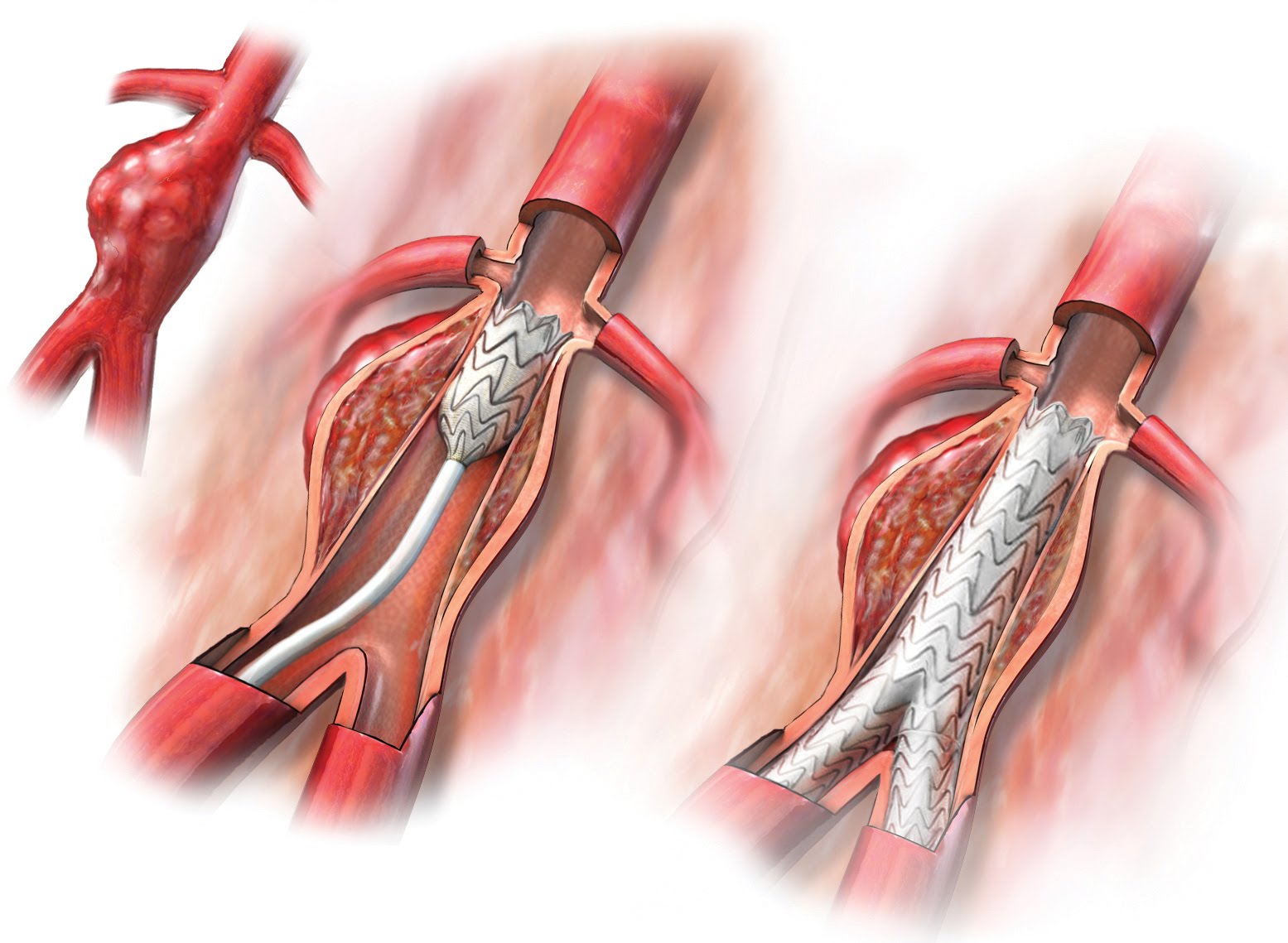
Therapy
Surgical therapy is mandatory, antibiotic therapy alone not being enough. General principles of the overall management strategies: Determining the extent of graft infection; ± removing the graft; Debridement of the arterial wall and perigraft tissues; Draining and antibiotic therapy.
Calligaro and colegues reccomended specific criteria for selective graft preservation:
• patent graft that is not construcetd of polyester:
• anastomoses are intact and not involved in the
infection;
• patient has no clinical signs of sepsis.