Acute pancreatitis is an inflammatory condition of the pancreas that is painful and at times deadly. Despite the great advances in critical care medicine over the past 20 years, the mortality rate of acute pancreatitis has remained at about 10%. Diagnosis of pancreatic problems is often difficult and treatments are therefore delayed because the organ is relatively inaccessible. There are no easy ways to see the pancreas directly without surgery, and available imaging studies are often inadequate. In addition to the acute form, there are hereditary and chronic forms of pancreatitis which can devastate a person over many years. Sufferers often endure pain and malnutrition, and are most likely left with a higher risk of pancreatic cancer.
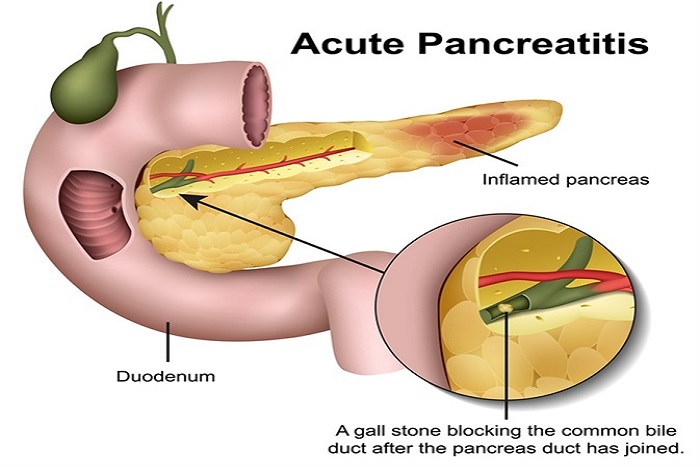
The most common cause of acute pancreatitis is stones in the gallbladder. Gallstones pass through the common bile duct to enter the small intestine. At the entry of the small intestine, the main pancreatic duct joins or lies immediately next to the common bile duct. It is believed that stones that get stuck in the common bile duct impinge on the main pancreatic duct, causing an obstruction of the normal flow of pancreatic fluid and leading to pancreatic injury. Another way that a stone can cause pancreatitis is by causing a backflow of bile into the pancreatic duct, resulting in pancreatic injury. Whereas the actual mechanism of how gallstones cause pancreatitis is not entirely certain, the association of gallstones and pancreatitis is clear.
There are several other causes of acute pancreatitis including:
Each year, there are more than 300,000 admissions to the hospital for treatment of acute pancreatitis, and the estimated cost of these admissions is greater than $2 billion. Between 16.5% and 25% of patients who develop acute pancreatitis experience a recurrent episode within the first several years. Preventing a recurrence is a major goal of treatment, with efforts focused on identifying the underlying cause and triggers to prevent future episodes.
Acute pancreatitis usually begins with gradual or sudden pain in the upper abdomen that sometimes extends to the back. The pain may be mild at first and become worse after eating. The pain is often severe, constant, and commonly lasts for several days in the absence of treatment. A person with acute pancreatitis usually looks and feels very ill and needs immediate medical attention. Most cases require hospitalization for 3 to 5 days for close monitoring, pain control, and intravenous hydration. Other symptoms can include:
Acute pancreatitis is confirmed by medical history, physical examination, and typically a blood test (amylase or lipase) for digestive enzymes of the pancreas. Blood amylase or lipase levels are typically elevated 3 times the normal level during acute pancreatitis. In some cases when the blood tests are not elevated and the diagnosis is still in question, abdominal imaging, such as a computed tomography (CT) scan, might be performed.
After diagnosis is confirmed, certain imaging tests might be performed during hospitalization or after to help identify the cause. Such tests include:
This is commonly performed during hospitalization to specifically evaluate the gallbladder for stones because gallstones are the most common cause of acute pancreatitis. Ultrasound uses sound waves that bounce off the pancreas, gallbladder, liver, and other organs, and their echoes generate electrical impulses that create an image—called a sonogram—on a video monitor. If gallstones are causing inflammation, the sound waves will also bounce off of them, showing their location.
This test is not commonly required during acute pancreatitis. Compared to transabdominal ultrasound, it is relatively more invasive, in that a physician passes a flexible thin tube down into the stomach. A camera and ultrasound probe are attached to the end of the tube, which enable the physician to look at images of the gallbladder, pancreas, and liver. The images are more sensitive than those of transabdominal ultrasound in detecting small stones in the gallbladder and bile ducts that may have been missed. It can also visualize the pancreas for abnormalities.
MRCP uses magnetic resonance imaging (MRI), a noninvasive procedure that produces cross-section images of parts of the body. After being lightly sedated, the patient lies in a cylinder-like tube. The technician injects dye into the patient’s veins, which helps show the pancreas, gallbladder, and pancreatic and bile ducts. This is another sensitive test for evaluating the gallbladder, bile ducts, and pancreas for causes of acute pancreatitis.
A CT scan is a noninvasive radiograph (x-ray) that produces 3-dimensional images of parts of the body. The patient lies on a table that slides into a donut-shaped machine. Typically not performed initially for an episode of acute pancreatitis, it may be performed when a diagnosis is uncertain or several days into hospitalization to evaluate the extent of pancreatic damage when a patient is not recovering as quickly as expected.
In most cases, acute pancreatitis resolves with therapy, but approximately 15% of patients develop severe disease.3 Severe acute pancreatitis can lead to life-threatening failure of multiple organs and to infection. Therefore, it is extremely important to seek medical attention if experiencing signs or symptoms of acute pancreatitis. Several clinical risk-scoring systems are available to help physicians predict who is most likely to develop severe acute pancreatitis. These scores rely on several pieces of clinical data collected at admission and during the first 48 hours of hospitalization. Commonly used scoring systems include:
One of the primary therapies for acute pancreatitis is adequate early fluid resuscitation, especially within the first 24 hours of onset. Pancreatitis is associated with a lot of swelling and inflammation. Giving fluids intravenously prevents dehydration and ensures that the rest of the organs of the body get adequate blood flow to support the healing process.
Initially, no nutrition is given to rest the pancreas and bowels during the first 24 to 48 hours. After 48 hours, a plan to provide nutrition should be implemented because acute pancreatitis is a highly active state of inflammation and injury that requires a lot of calories to support the healing process. In most cases, patients can start to take in food on their own by 48 hours. If this is not possible, then a feeding tube that is passed through the nose into the intestines can be used to provide nutrition. This method is safer than providing nutrition intravenously. There is no benefit to using probiotics for acute pancreatitis.
Intravenous medications, typically potent narcotic pain medications, are effective in controlling pain associated with acute pancreatitis. Nausea is a common symptom and can be due to pancreatic inflammation as well as slowing of the bowels. Effective intravenous medications are available for nausea. Pain and nausea will decrease as the inflammation resolves.
In addition to providing supportive care, underlying causes need to be promptly evaluated. If the acute pancreatitis is thought to be due to gallstones, medication, high triglycerides, or high calcium levels within the patient’s body (or other external causes), directed therapy can be implemented.
ERCP is a procedure in which a physician with specialized training passes a flexible, thin tube with a camera attached to the end through the patient’s mouth and into the first part of the small intestine, where the bile duct and pancreatic duct exit. With this device, a small catheter can be passed into the bile duct to remove gallstones that might have gotten stuck and are the cause of pancreatitis. In certain situations, a special catheter can also be passed into the pancreatic duct to help the pancreas heal.
The Following Procedures can be Performed With ERCP:
SPHINCTEROTOMY
Using a small wire on the endoscope, a physician finds the muscle that surrounds the pancreatic duct or bile duct and makes a tiny cut to enlarge the duct opening. When a pseudocyst is present, the duct is drained.
GALLSTONE REMOVAL
The endoscope is used to remove pancreatic or bile duct stones with a tiny basket. Gallstone removal is sometimes performed along with a sphincterotomy.
STENT PLACEMENT
Using the endoscope, a physician places a tiny piece of plastic or metal that looks like a straw into a narrowed pancreatic or bile duct to keep it open.
BALLOON DILATATION
Some endoscopes have a small balloon that a physician uses to dilate, or stretch, a narrowed pancreatic or bile duct. A temporary stent can be placed for a few months to keep the duct open.
It is well documented that one of the main side effects of ERCP is pancreatitis; however, there are several clearly defined situations when urgent ERCP is indicated for acute pancreatitis.
Basic and clinical evidence suggests that the development of both acute pancreatitis (AP) and chronic pancreatitis (CP) can be associated with oxidative stress. Findings show that free radical activity and oxidative stress indices are higher in the blood and duodenal juice of patients with pancreatitis.
Based on these findings, the idea of using antioxidant regimens in the management of both AP and CP as a supplement and complementary in combination with its traditional therapy is reasonable. In practice, however, the overall effectiveness of antioxidants is not known, and the best mixture of agents and dosages is not clear. Currently, a trial of a mixture of antioxidants containing vitamin C, vitamin E, selenium, and methionine is reasonable as one component of overall medical management.
In summation, there is no definite consensus on the dosage, length of therapy, and ultimately, the benefits of antioxidant therapy in the management of AP or CP. Further well-designed clinical studies are needed to determine the appropriate combination of agents, time of initiation, and duration of therapy.
NECROTIZING PANCREATITIS:
The definition of severe acute pancreatitis includes cases in which a portion of pancreatic tissue is no longer viable because of injury—this is called necrosis. Over time, the body will resorb this dead tissue. In some cases, this dead tissue can become a source of infection. When infection is suspected, diagnosis can be made by needle biopsy, and if confirmed, medical treatment with antibiotics is required along with consideration of drainage.