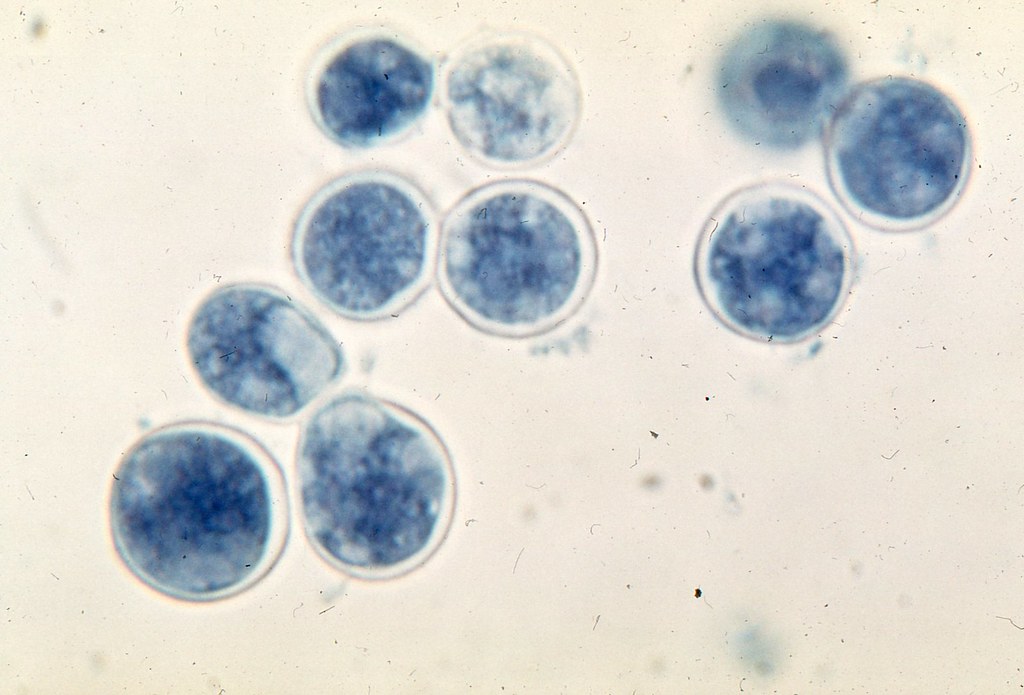
Blastomycosis is a systemic pyogranulomatous infection usually caused by the inhalation of (spores) conidia of Blastomyces dermatitidis. Clinical presentations vary widely, ranging from an asymptomatic, self-limited pulmonary infection to acute respiratory distress syndrome (ARDS), a life-threatening disease.
Blastomycosis is usually localized to the lungs and may present with:
A self-limited flulike illness with fever, chills, myalgia, headache, and a nonproductive cough
An acute illness resembling bacterial pneumonia, with high fever, chills, a productive cough, and pleuritic chest pain; mucopurulent or purulent sputum
Chronic illness, with low-grade fever, a productive cough, fatigue, night sweats, and weight loss
Rapidly progressive, and severe disease, eg, multilobar pneumonia or ARDS, with fever, shortness of breath, tachypnea, hypoxemia, and finally hemodynamic collapse
Extrapulmonary manifestations are present in 25-40% of cases and may present with:
Cutaneous lesions – Usually either verrucous or ulcerative and may be asymptomatic
Osteoarticular lesions – Cause bone or joint pain; soft-tissue swelling possible; possible involvement of any bone may be involved, but the vertebrae and pelvis are common sites
Genitourinary manifestations including prostatitis and epididymitis – May be asymptomatic or may cause pain on urinating
Other sites – Blastomycosis dermatitidis has been reported to involve almost all organs including the eye, liver, sleep, breast, thyroid, and adrenal gland.
Central nervous system involvement – Intracranial or epidural abscesses and meningitis
Diagnostic studies include the following:
Sputum specimens processed with 10% potassium hydroxide, cytology smears, or a fungal stain
Culture of sputum or tissue specimens
Enzyme immunoassay (EIA) techniques on sputum, tissue, or bronchoscopic specimens
Imaging studies (eg, chest radiography, CT, MRI)
Antifungal treatment is as follows:
Treatment
Patients with a subclinical disease (presence of serologic or other markers without symptoms) can be observed and do not require antifungal treatment. Mild to moderate disease should be treated in all patients. All immunocompromised patients and patients with progressive pulmonary disease or extrapulmonary disease require treatment.
Therapeutic approaches have evolved in recent years with the advent of oral azoles, primarily itraconazole, which has replaced amphotericin B for mild-to-moderate pulmonary blastomycosis in adult patients, and is used for completion of therapy after initial amphotericin treatment in more severe cases. Voriconazole may have a role in the treatment of CNS blastomycosis.
The need for inpatient and intensive care unit (ICU) care is based on the acuity and pace of the disease progression as well as the immune status of the patient. Admit severely and progressively ill patients to the ICU, including those with acute respiratory distress syndrome (ARDS).
Inpatient care often is needed for workup and treatment of blastomycosis presenting as an undiagnosed pneumonia, for pleural effusion, and for extrapulmonary manifestations such as meningitis. In addition, initiation of amphotericin B treatment is preferably performed in an inpatient setting (ie, with infusion through an indwelling central venous line in an observation room with a trained staff).