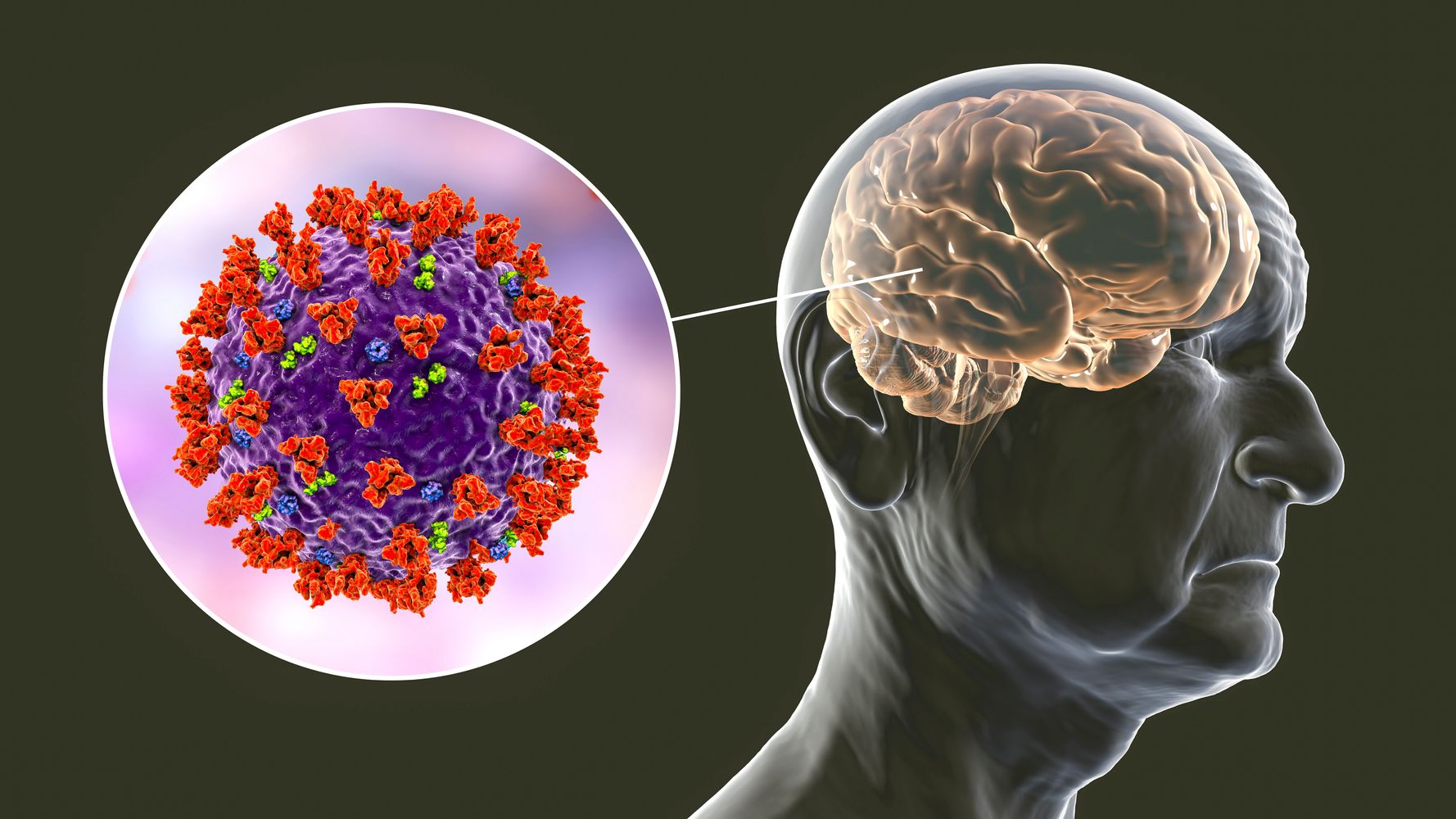
Meningitis is an inflammation of the membranes (meninges) surrounding your brain and spinal cord.
The swelling from meningitis typically triggers symptoms such as headache, fever and a stiff neck.
Most cases of meningitis in the United States are caused by a viral infection, but bacterial, parasitic and fungal infections are other causes. Some cases of meningitis improve without treatment in a few weeks. Others can be life-threatening and require emergent antibiotic treatment.
Seek immediate medical care if you suspect that someone has meningitis. Early treatment of bacterial meningitis can prevent serious complications.
Many different viruses can cause meningitis. Most people are exposed to some of them during their life without developing meningitis. The most common causes are:
Coxsackie or Echovirus groups of enteroviruses are the most common cause of viral meningitis. Most infections produce no symptoms, or mild symptoms such as sore throats, colds and flu-like illnesses. Some of them may also cause stomach upsets and diarrhoea.
Enteroviruses mostly affect children, who are the main transmitters of these viruses.
Enteroviral infections are prevalent in the UK during summer and autumn months. Spread is mainly by hand to mouth transmission.
Herpes viruses are the other common cause of viral meningitis in adolescents and adults in developed countries[2]. Herpes viruses include the herpes simplex viruses (HSVs) and varicella zoster virus – the same virus that causes chickenpox and shingles.
HSVs can cause meningitis or encephalitis (inflammation of the brain itself, which is much more serious). HSV encephalitis is mainly caused by HSV-1 (which is also the cause of most cold-sores), whereas meningitis is more often caused by HSV-2 (more often a cause of genital herpes). HSV viruses have been linked to Recurrent Lymphocytic Meningitis, also known as Mollaret’s meningitis. It is characterised by sudden attacks of meningitis symptoms that usually last for 2-7 days and are separated by symptom free intervals lasting for weeks,months or years.
HSV-1 and -2 infections are very common but most people affected have only minor symptoms or no symptoms at all. Transmission is via contact with an infected area of the skin when the virus is active. HSV-1 is usually acquired orally during childhood and about 6 out of 10 people in the UK carry it. HSV-2 is primarily a sexually transmitted infection and is carried by about 1 in 10 of the UK population[3]. Many people harbour HSV without ever knowing they have it. Since they can transmit the virus without having symptoms, infection can be spread unknowingly to contacts. The timing of transmission is unpredictable, so genital herpes infection (and herpes meningitis) can appear even after many years in a monogamous relationship.
VZV meningitis can occur at the same time as chickenpox or shingles or it can occur in its own without any rash or skin manifestation.
Other Herpes viruses are less frequent causes of meningitis compared to HSV and VZV.
Before MMR vaccine was available, mumps was the most common cause of viral meningitis in the UK and occurred in 15% of patients with mumps[4]. A recent resurgence in cases in the UK largely affected late teenagers and young adults who did not receive a full course of measles-mumps-rubella (MMR) vaccine[1]. Measles can also cause meningitis and encephalitis.
Flaviviruses
These viruses normally affect wild animals such as birds or rodents and are carried by mosquitoes or ticks. Some of these viruses such as West Nile virus, Japanese B encephalitis and tick-borne encephalitis can cause meningitis or encephalitis in humans but this is not a problem in the UK and Ireland.
Human immunodeficiency virus (HIV) can cause meningitis during the early stages of HIV infection. In cases of viral meningitis it is not always possible to identify the type of virus responsible for the disease (approximately 30-40% of patients have no pathogen identified). Although HIV is a rare cause of viral meningitis, it is important that adults with viral meningitis due to unknown cause undergo an HIV test. This is because viral meningitis may be the first sign of infection with HIV and if it is not identified at this early stage then it may remain symptomless and undiagnosed until the individual has advanced disease or AIDS. It is hoped that by screening such cases more individuals with HIV will be identified and treated early resulting in better outcomes.
Your family doctor or pediatrician can diagnose meningitis based on a medical history, a physical exam and certain diagnostic tests. During the exam, your doctor may check for signs of infection around the head, ears, throat and the skin along the spine.
You or your child may undergo the following diagnostic tests:
CSF analysis may also help your doctor identify which bacterium caused the meningitis. If your doctor suspects viral meningitis, he or she may order a DNA-based test known as a polymerase chain reaction (PCR) amplification or a test to check for antibodies against certain viruses to determine the specific cause and determine proper treatment.
Acyclovir can be used to treat HSV infection. However, there are no effective therapies for most viruses that cause meningitis (antibiotics are ineffective against viruses), so treatment is normally limited to easing the symptoms of the disease (for example painkillers for headache or anti-emetics to stop vomiting). Most people recover without any medical treatment within 5 days to a fortnight, but for some the recovery period is more prolonged.
The doctor may do a lumbar puncture. This is when a sample of cerebrospinal fluid (CSF) is taken from the spinal canal (the passageway through the back bones which contains the spinal cord). The sample of CSF will be examined and then sent for further laboratory testing. A lumbar puncture is important to confirm the diagnosis of meningitis, and to show which germ is causing the illness.
What after effects can viral meningitis cause?
Most people recover with no noticeable effects, however recent studies have found that some patients with viral meningitis may develop short-term memory loss and attention deficits[5-6]. There is also some evidence that children who have viral meningitis under 1 year of age, may develop subtle neurological problems later in life[7].
Am I at risk of spreading or contracting the disease if I have been in contact with a patient with viral meningitis?
The risk to contacts is very low. Viral meningitis does not normally require public health measures to be taken because although some of the viruses that cause it are contagious, most people infected have no symptoms, or only very mild ones. A person with viral meningitis may pass on the virus, but this would be very unlikely to cause another person to develop viral meningitis as well.
Most causes of viral meningitis are not preventable, although a good general precaution against viral meningitis is attention to handwashing since enteroviruses in particular usually enter the body via the hand to mouth route. Immunisation against mumps and measles (MMR) is offered to children at 12-13 months and 3 years of age as part of the routine childhood immunisation schedule. Immunisations are also available for some Flaviviruses such as tick-borne encephalitis and Japanese encephalitis, and are recommended for travellers to areas where the risk of these infections is high.