Hepatitis C is a contagious, viral liver disease. It is the most common blood-borne disease in the United States, and most people with hepatitis C do not realize that they have it.
The disease spreads by blood-to-blood contact, and primarily by the use of injectable drugs. There are immunizations against hepatitis A and B, but not C. To prevent infection, it is necessary to avoid exposure to the hepatitis C virus (HCV).
If the virus does not clear within six months, the infection becomes chronic and only curable with medication. HCV can result in scarring, cirrhosis, cancer of the liver, and in some cases, death. There are, however, new medications that can cure chronic hepatitis C infection.
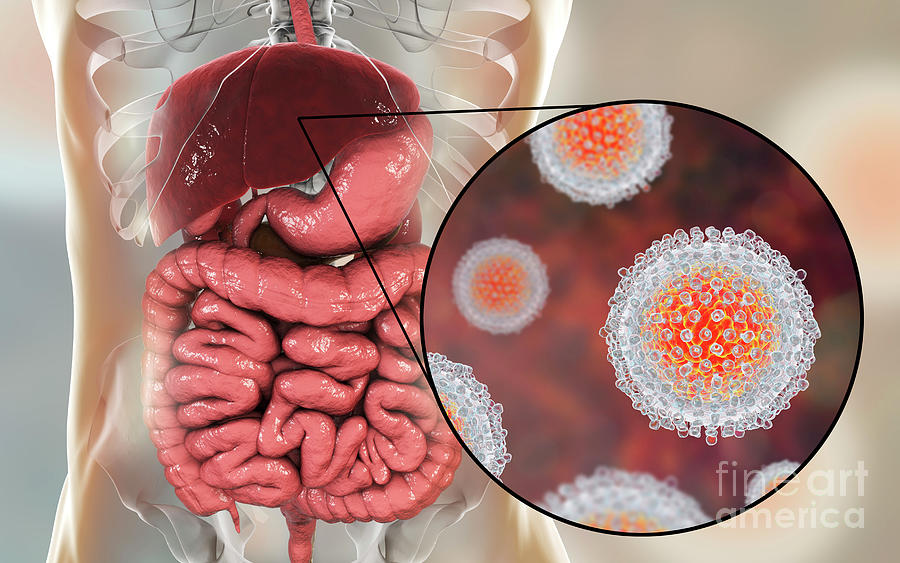
HCV is a virus that damages the liver.
Hepatitis is an inflammation of the liver. There are several strains of viral hepatitis. The most common types are A, B, and C.
The virus invades the cells in the liver and causes swelling and dysfunction.
There is no vaccination for HCV. The presence of HCV antibodies in the immune system does not provide long-term protective immunity in the same way as a vaccine. The immune system holds no permanent record of HCV antibodies.
A person can become re-infected with a different strain of the virus.
HCV often does not present symptoms at its acute stage. However, the condition can escalate to a chronic stage at which potentially fatal complications can develop.
Acute HCV infection is rarely diagnosed due to the lack of definitive symptoms. It is often referred to as a silent epidemic. The average time frame from exposure to noticeable symptoms is between 4 and 15 weeks.
During this acute period, symptoms will not seem different to those caused by any other viral syndrome. People with acute HCV will experience:
HCV becomes chronic when the virus remains in the blood for six months after the acute infection period. If the presence of HCV viruses is detected in testing at least twice over this period, a chronic diagnosis is confirmed.
The infection will not resolve unless treated with medication.
Most people experience no symptoms with chronic HCV infection. Some may experience ongoing episodes of abdominal pain, persistent fatigue, and aching joints.
After 25 to 30 years, this chronic infection may result in significant scarring, or fibrosis, of the liver. If the entire liver becomes scarred, this can progress to cirrhosis, liver failure, and possibly liver cancer.
The overall health of the infected individual and their liver will determine how quickly damage and possible progression to cirrhosis will occur. The genotype of the virus plays less of a role than the physical health of the person with HCV.
The HCV virus causes hepatitis C. The virus is transmitted through blood-to-blood contact.
Viruses are inactive until they enter the living cell of a host. They will then hijack the hardware of the cell to make copies of themselves. Chronic HCV infection consists of millions, or possibly billions, of copies of the virus circulating within the body.
For a blood-to-blood infection to occur, blood from an infected person must enter the body of someone who is not infected. The biggest risk factor for becoming infected with HCV is sharing needles or equipment used to inject drugs.
HCV is not transmitted through casual contact, respiratory droplets, sharing food, kissing, or mosquito bites.
A speck of blood so small that it is not viewable to the naked eye can carry hundreds of hepatitis C virus particles. Cleaning a needle with alcohol, rinsing it with soap and water will not kill the virus.
Once the virus is injected into the body, even if on only one occasion, exposure has occurred and infection is possible. Injecting drugs causes approximately 67 percent of global cases.
The Centers for Disease Control (CDC) have identified the factors that lead to the greatest risk of HCV exposure. These include:
People who are at risk due to these factors can receive a screening to rule out HCV.
HCV is often overlooked or mistaken for a less severe viral illness. It is rare for the infection to be diagnosed during the acute phase.
The immune system of a person infected with HCV responds to the infection and, in only 20 percent of cases, will clear the virus without assistance. The remaining 80 percent of cases will turn chronic, and it can become possible to spread HCV to others without knowing.
Screening tests are available for people the CDC have determined are at risk. People can test for HCV using a simple blood test called an HCV antibody screen.
There is a rapid test approved by the Food and Drug Administration (FDA) that provides results in 20 minutes. Otherwise, the blood is drawn from a vein and processed at a lab. A negative test means that the person has not been exposed. A positive test means that the person has been exposed to HCV, but does not necessarily prove ongoing infection.
All positive HCV antibody results will lead to a second blood test called HCV RNA (PCR). This test will demonstrate whether the virus is still present.
A person with a positive PCR should see a liver specialist or a provider trained to treat HCV.
It is important to note that the positive antibody test will always remain positive, whether or not the virus is still present.
Once the chronic infection is confirmed, the genotype of the virus is established by testing. This will determine the percentile cure rate, the length of treatment, and the preferred medications.
In some instances, a liver biopsy may be recommended for grading the severity of the disease, staging the degree of fibrosis, and evaluating the extent of liver damage.
Treatment of HCV removes the viruses from the body.
The current treatment for chronic hepatitis C is a combination of medications.
The choice of medication and duration of treatment depends on the genotype of the virus. Genotype 1a is the most prevalent in the US, and presently there are several recommended treatment options using a combination of powerful antiviral medications.
Direct-acting antivirals (DAAs) are the newest available agents to treat HCV. These medications work by targeting specific steps in the HCV life cycle to disrupt the reproduction of viral cells.
Before the availability of DAAs, the treatment for chronic HCV was lengthy and uncomfortable, with less than ideal cure rates. Now the cure rates are over 90 percent. The average duration of treatment is 8 to 12 weeks. The medications are well-tolerated, with the most common side effects being headache and fatigue.
Preventing HCV involves limiting exposure to the virus in the first instance.
Because HCV can only be transmitted through blood to infected blood exposure, the number one way to prevent spreading HCV is by not sharing needles and avoiding all contact with the blood of other people.
[caption id="attachment_349" align="alignright" width="325"] https://www.youtube.com/watch?v=vqvSG9hqGUs -For this video[/caption]
Once identified, people infected with HCV should receive both the hepatitis A and B vaccines, and make lifestyle changes to promote optimum liver health.
Obesity, smoking, diabetes and alcohol consumption can accelerate the rate of liver scarring. It is important that all individuals with HCV infection maintain good health. This involves: