Rheumatic fever is an inflammatory disease that can develop as a complication of inadequately treated strep throat or scarlet fever. Strep throat and scarlet fever are caused by an infection with streptococcus bacteria.
Rheumatic fever is most common in 5- to 15-year-old children, though it can develop in younger children and adults. Although strep throat is common, rheumatic fever is rare in the United States and other developed countries. However, rheumatic fever remains common in many developing nations.
Rheumatic fever can cause permanent damage to the heart, including damaged heart valves and heart failure. Treatments can reduce damage from inflammation, lessen pain and other symptoms, and prevent the recurrence of rheumatic fever.
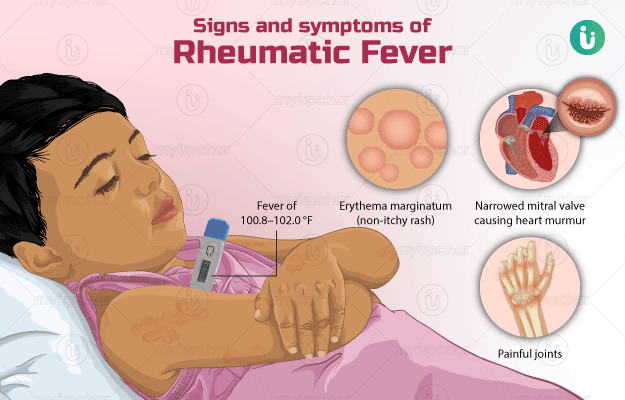
Rheumatic fever symptoms vary. You can have few symptoms or several, and symptoms can change during the course of the disease. The onset of rheumatic fever usually occurs about two to four weeks after a strep throat infection.
Rheumatic fever signs and symptoms — which result from inflammation in the heart, joints, skin or central nervous system — can include:
Rheumatic fever can occur after an infection of the throat with a bacterium called group A streptococcus. Group A streptococcus infections of the throat cause strep throat or, less commonly, scarlet fever. Group A streptococcus infections of the skin or other parts of the body rarely trigger rheumatic fever.
The link between strep infection and rheumatic fever isn't clear, but it appears that the bacterium tricks the immune system. The strep bacterium contains a protein similar to one found in certain tissues of the body. So immune system cells that would normally target the bacterium may treat the body's own tissues as if they were infectious agents — particularly tissues of the heart, joints, skin and central nervous system. This immune system reaction results in inflammation.
If your child receives prompt treatment with an antibiotic to eliminate strep bacteria and takes all medication as prescribed, there's little chance of developing rheumatic fever. If your child has one or more episodes of strep throat or scarlet fever that aren't treated or not treated completely, he or she might develop rheumatic fever.
Factors that can increase the risk of rheumatic fever include:
Inflammation caused by rheumatic fever can last a few weeks to several months. In some cases, the inflammation causes long-term complications.
Rheumatic heart disease is permanent damage to the heart caused by rheumatic fever. It usually occurs 10 to 20 years after the original illness. Problems are most common with the valve between the two left chambers of the heart (mitral valve), but the other valves can be affected. The damage can result in:
Damage to the mitral valve, other heart valves or other heart tissues can cause problems with the heart later in life. Resulting conditions can include:
The only way to prevent rheumatic fever is to treat strep throat infections or scarlet fever promptly with a full course of appropriate antibiotics.
Although there's no single test for rheumatic fever, diagnosis is based on medical history, physical exam and certain test results.
If your child was already diagnosed with a strep infection, your doctor might not order additional tests for the bacterium. If your doctor orders a test, it will most likely be a blood test that can detect antibodies to the strep bacterium circulating in the blood. The actual bacterium might no longer be detectable in your child's throat tissues or blood.
Your doctor also is likely to check for inflammation in your child's blood by measuring C-reactive protein and the erythrocyte sedimentation rate.
This test — also called an ECG or EKG — records electrical signals as they travel through your child's heart. Your doctor can look for patterns among these signals that indicate inflammation of the heart or poor heart function.
Using sound waves to produce live-action images of the heart, this test can enable your doctor to detect heart abnormalities.
The goals of treatment for rheumatic fever are to destroy remaining group A streptococcal bacteria, relieve symptoms, control inflammation and prevent recurrences.
Treatments include:
After your child has completed the full antibiotic treatment, your doctor will begin another course of antibiotics to prevent recurrence of rheumatic fever. Preventive treatment will likely continue through age 21 or until your child completes a minimum five-year course of treatment, whichever is longer.
People who have had heart inflammation during rheumatic fever might be advised to take the preventive antibiotic treatment for 10 years or longer.